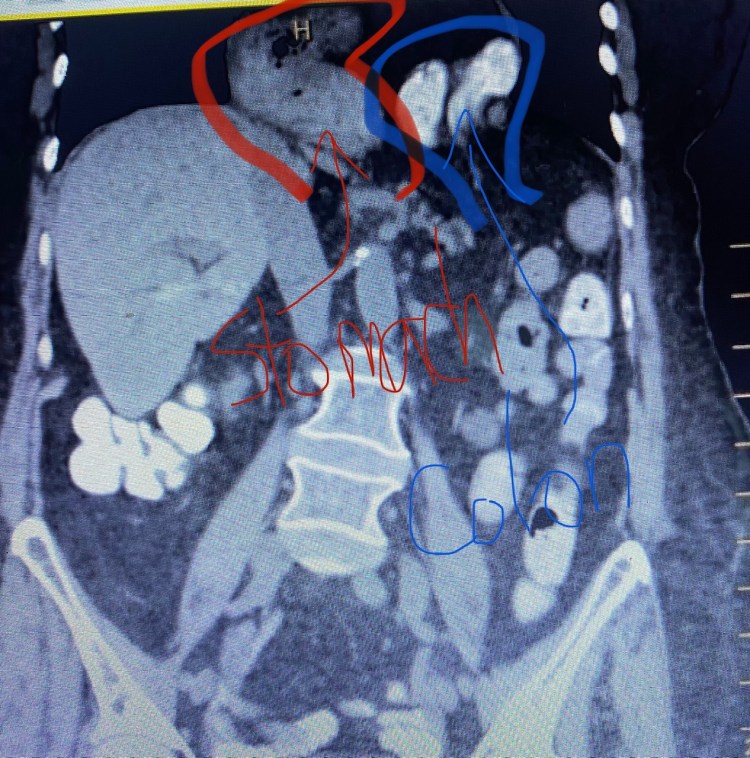
Figure 1. Weekly cancer screening volume vs. week number in year for each type of cancer screening. Colored capsules show the last observed volume.
Some key findings in the WSJ report illustrate the scale of delayed or missed cancer detection:
- UnitedHealth Group claims data shows mammograms fell by as much as 95 percent in the second week of April compared with that same week in years prior.
- UnitedHealth’s count shows nearly 1 million fewer mammograms, colorectal and cervical cancer screenings performed in the first eight months of 2020 compared with the same period last year.
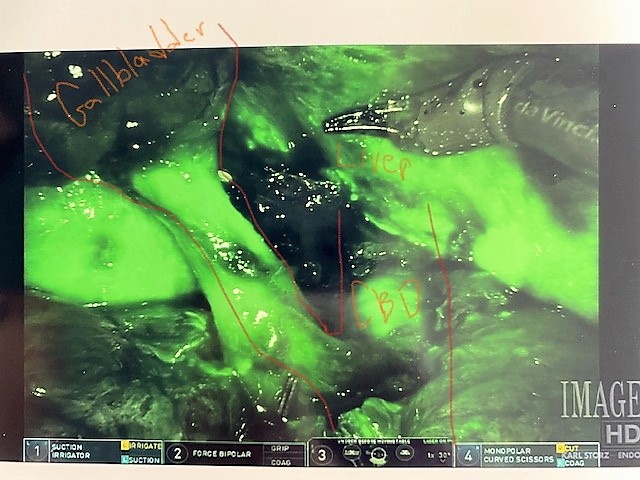
- With 300 sites of care across the U.S., cancer care network 21st Century Oncology said about 18 percent of newly diagnosed breast cancer patients this year through August had an advanced stage of the disease compared with 12 percent in all of 2019. A C-level leader told the WSJ the trend is “distressing as a physician.”
- Quest Diagnostics’ data shows the mean weekly number of newly detected cases of several types of cancer dropped sharply this spring, including a 52 percent drop for breast cancer in March and early April compared with detection figures before the pandemic. Wall Street Journal reports.